Abstract
Objective
Granuloma etiology includes infections, vasculitis, chemicals, malignancies, lymphoproliferative disorders, and immunological diseases. We hypothesized that patients with granuloma have an underlying primary immunodeficiency disease (PIDD).
Patients and Methods
We retrospectively enrolled 82 patients with immunological evaluation among 294 biopsy-proven granuloma patients (0- to 20-year-old). At the same time frame, we followed up with 1910 patients in the same age group.
Results
Out of 82 patients, male/female ratio was 45/37. Median age at symptom onset was 5 years (28 days–17.4 years), age of granuloma at diagnosis was 8.6 years (36 days–19.4 years). Common symptoms at disease onset were fever (23.2%), lymphadenopathy (19.6%), abdominal pain (12.2%), and cough (12.2%). Granuloma was frequent in lymph nodes (26.8%), skin (19.5%), lung (13.4%), and bone (11%). Common infectious agents isolated were Mycobacterium spp. (23.2%) and EBV (4.9%).
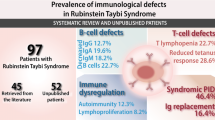
We document PIDD in 76.8% (63/82) of patients. 49.4% (40/81) of immunologically evaluated granuloma patients had hypogammaglobulinemia. Granuloma rate in pediatric PIDD was 3.3%(63/1910).
Patients with multiple granulomas (n = 16) had a PIDD diagnosis. Lung involvement was three times more in PIDD. Brain involvement was only seen in PIDD. Fibroadipose tissue and liver involvement were more frequent in patients without documented PIDD and patients whose evaluation was not completed.
The mortality rate in PIDD with granuloma was 15.9%, whereas there was no mortality in patients without PIDD.
Conclusion
As documented here, even in a university hospital, the immunologic evaluation ratio is about one-third. We showed high PIDD frequency in children with granuloma, and higher mortality in PIDD with granuloma. Thus, an immunologic evaluation performed meticulously by immunologists is a must for accurate diagnosis and decision of individualized therapeutic options.



Similar content being viewed by others
Data Availability
On a reasonable request, the data supporting study’s findings are available from the corresponding author.
References
Bousfiha A, Jeddane L, Picard C, et al. Human Inborn Errors of Immunity: 2019 Update of the IUIS Phenotypical Classification. J Clin Immunol. 2020;40:66–81.
Tangye SG, Al-Herz W, Bousfiha A, et al. Human Inborn Errors of Immunity: 2019 Update on the Classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol. 2020;40:24–64. https://doi.org/10.1007/s10875-019-00737-x.
Al-Muhsen SZ. Gastrointestinal and hepatic manifestations of primary immune deficiency diseases. Saudi J Gastroenterol. 2010;16:66–74. https://doi.org/10.4103/1319-3767.61230.
Leung J, Sullivan KE, Perelygina L, Icenogle JP, Fuleihan RL, Lanzieri TM. Prevalence of granulomas in patients with primary ımmunodeficiency disorders, United States: data from National Health Care Claims and the US Immunodeficiency Network Registry. J Clin Immunol. 2018;38:717–26.
Siegfried EC, Prose NS, Friedman NJ, Paller AS. Cutaneous granulomas in children with combined immunodeficiency. J Am Acad Dermatol. 1991;25:761–6.
Keczkes K, Bilimoria S, Piercy DM. Pernicious anaemia and granulomatous skin lesions in a case of common variable hypogammaglobulinaemia. Br J Dermatol. 1979;101:211–7.
Paller AS, Massey RB, Curtis MA, et al. Cutaneous granulomatous lesions in patients with ataxiatelangiectasia. J Pediatr. 1991;119:917–22.
Fleming MG, Gewurz AT, Pearson RW. Caseating cutaneous granulomas in a patient with Xlinked infantile hypogammaglobulinemia. J Am Acad Dermatol. 1991;24:629–33.
Pierson JC, Camisa C, Lawlor KB, Elston DM. Cutaneous and visceral granulomas in common variable immunodeficiency. Cutis. 1993;52:221–2.
Harp J, Coggshall K, Ruben BS, Ramírez-Valle F, He SY, Berger TG. Cutaneous granulomas in the setting of primary immunodeficiency: a report of four cases and review of the literature. Int J Dermatol. 2015;54:617–25.
Petersen HJ, Smith AM. The role of the innate immune system in granulomatous disorders. Front Immunol. 2013;4:120.
Ramakrishnan L. Revisiting the role of the granuloma in tuberculosis. Nat Rev Immunol. 2012;12:352–66.
Kumar V, Abul KA, and Aster JC. Robbins and Cotran pathologic basis of disease. Ninth edition. Philadelphia, PA: Elsevier/Saunders. 2015.
James DG. A clinicopathological classification of granulomatous disorders. Postgrad Med J. 2000;76:457–65.
Shah KK, Pritt BS, Alexander MP. Histopathologic review of granulomatous inflammation. J Clin Tuberc Other Mycobact Dis. 2017;7:1–12. https://doi.org/10.1016/j.jctube.2017.02.001.
Bodemer C, Sauvage V, Mahlaoui N, et al. Live rubella virus vaccine long-term persistence as an antigenic trigger of cutaneous granulomas in patients with primary immunodeficiency. Clin Microbiol Infect. 2014;20:O656–63. https://doi.org/10.1111/1469-0691.12573.
Koçali B., Evaluating the diagnosis and clinical features of the patients who followed up with primary ımmunodeficiency diagnosis in Hacettepe University İhsan Doğramacı Children’s Hospital Pediatric Immunology Department, Hacettepe University Faculty of Medicine Department of Pediatrics, Thesis in Pediatrics, Ankara. 2020.
Backeljauw P, Cappa M, Kiess W, et al. Impact of short stature on quality of life: A systematic literature review. Growth Horm IGF Res. 2021;101392:57–8. https://doi.org/10.1016/j.ghir.2021.101392.
Shearer WT, Rosenblatt HM, Gelman RS, et al. Lymphocyte subsets in healthy children from birth through 18 years of age: the Pediatric AIDS Clinical Trials Group P1009 study. J Allergy Clin Immunol. 2003;112:973–80. https://doi.org/10.1016/j.jaci.2003.07.003.
Piątosa B, Wolska-Kuśnierz B, Pac M, Siewiera K, Gałkowska E, Bernatowska E. B cell ubsets in healthy children: reference values for evaluation of B cell maturation process in peripheral blood. Cytometry B Clin Cytom. 2010;78:372–81. https://doi.org/10.1002/cyto.b.20536.
Ekinci A., Evaluation and comparison of peripherale blood lymphocyte functions in healty children by using two different methods, Ankara Unıversıty Bıotechnology Instıtute, Postgraduate Thesis, Ankara, 2006.
Schatorjé EJ, Gemen EF, Driessen GJ, Leuvenink J, van Hout RW, de Vries E. Paediatric reference values for the peripheral T cell compartment. Scand J Immunol. 2012;75:436–44. https://doi.org/10.1111/j.1365-3083.2012.02671.x.
Moraes-Pinto MI, Ono E, Santos-Valente EC, et al. Lymphocyte subsets in human immunodeficiency virus-unexposed Brazilian individuals from birth to adulthood. Mem Inst Oswaldo Cruz. 2014;109:989–98. https://doi.org/10.1590/0074-0276140182.
Rose CD, Neven B, Wouters C. Granulomatous inflammation: the overlap of immune deficiency and inflammation. Best Pract Res Clin Rheumatol. 2014;28:191–212.
https://asi.saglik.gov.tr/asi-takvimi2. (Access 01 July 2022)
Chiam LY, Verhagen MM, Haraldsson A, et al. Cutaneous granulomas in ataxia telangiectasia and other primary immunodeficiencies: reflection of inappropriate immune regulation? Dermatology (Basel, Switzerland). 2011;223:13–9.
Zumla A, James DG. Granulomatous infections: etiology and classification. Clin Infect Dis. 1996;23:146–58. https://doi.org/10.1093/clinids/23.1.146.
https://apps.who.int/iris/rest/bitstreams/1379788/retrieve. (Access 09 May 2022).
Doğru D, Kiper N, Ozçelik U, Yalçin E, Tezcan I. Tuberculosis in children with congenital immunodeficiency syndromes. Tuberkuloz ve toraks. 2010;58:59–63.
Donald PR. Childhood tuberculosis: out of control? Curr Opin Pulm Med. 2002;8:178–82. https://doi.org/10.1097/00063198-200205000-00005.
Chiang SS, Swanson DS, Starke JR. New diagnostics for childhood tuberculosis. Infect Dis Clin North Am. 2015;29:477–502.
Seger RA. Advances in the diagnosis and treatment of chronic granulomatous disease. Curr Opinion Hematol. 2011;18.
Barkai T, Somech R, Broides A, et al. Late diagnosis of chronic granulomatous disease. Clin Exp Immunol. 2020;201:297–305.
Falcone EL, Zelazny AM, Holland SM. Rothia aeria neck abscess in a patient with chronic granulomatous disease: case report and brief review of the literature. J Clin Immunol. 2012;32:1400–3.
Morgan EA, Henrich TJ, Jarell AD, et al. Infectious granulomatous dermatitis associated with Rothia mucilaginosa bacteremia: a case report. Am J Dermatopathol. 2010;32:175–9.
Tsukamoto N, Handa H, Yokohama A, et al. Long-term follow-up of EBV-positive lymphoproliferative disorders in a patient with systemic lupus erythematosus. Med Mol Morphol. 2011;44:237–41.
Gangar P, Venkatarajan S. Granulomatous lymphoproliferative disorders: granulomatous slack skin and lymphomatoid granulomatosis. Dermatol Clin. 2015;33:489–96.
Reyes C, Abuzaitoun O, De Jong A, Hanson C, Langston C. Epstein-Barr virus-associated smooth muscle tumors in ataxia-telangiectasia: a case report and review. Hum Pathol. 2002;33:133–6.
McClain KL, Leach CT, Jenson HB, et al. Association of Epstein-Barr virus with leiomyosarcomas in young people with AIDS. N Engl J Med. 1995;332:12–8.
Ardeniz O, Cunningham-Rundles C. Granulomatous disease in common variable immunodeficiency. Clin Immunol (Orlando, Fla). 2009;133:198–207.
Mullighan CG, Fanning GC, Chapel HM, Welsh KI. TNF and lymphotoxin-alpha polymorphisms associated with common variable immunodeficiency: role in the pathogenesis of granulomatous disease. J Immunol. 1997;159:6236–41.
Kliegman R. Nelson Textbook of Pediatrics. Edition 21. Philadelphia, PA: Elsevier. 2020.
Gadola SD, Moins-Teisserenc HT, Trowsdale J, Gross WL, Cerundolo V. TAP deficiency syndrome. Clin Exp Immunol. 2000;121:173–8.
Caka C, Cimen O, Kahyaoğlu P, Tezcan İ, Cagdas D. Selective IgM deficiency: follow-up and outcome. Pediatr Allergy Immunol. 2021;32:1327–34.
van Stigt AC, Dik WA, Kamphuis LSJ, et al. What works when treating granulomatous disease in genetically undefined CVID? A Syst Rev Front Immunol. 2020;11:606389.
Gerke AK. Treatment of Sarcoidosis: A Multidisciplinary Approach. Front Immunol. 2020;11:545413.
https://cci-reporting.uniklinik-freiburg.de/#/. (Access 09 October 2021).
https://usidnet.org/registry-data/stats-registry-enrollment. (Access 09 October 2021).
Acknowledgements
The authors thank the patient’s family and all the medical teams involved for their cooperation.
Author information
Authors and Affiliations
Contributions
MS collected the data and participated in the review of the files, data generation, entry, and analysis, and wrote the manuscript. OS collected the data and participated in the review of the files, data generation, entry and analysis. BK collected the data and participated in the review of files and data generation. DO, MC, EEY, UÖ, NK, İT, and DDE contributed to patient screening, collection of the data, data generation, data analysis, and interpretation of the results. DC planned the study; contributed to patient screening, collection of the data, data generation, data analysis, and interpretation of the results; and wrote the manuscript with MS. All of the authors reviewed it critically for important intellectual content and agreed to be accountable for all aspects of the work related to its accuracy or integrity.
Corresponding author
Ethics declarations
Ethics Approval
Ethics committee approval was received for this study from the Hacettepe University Non-Invasive Clinical Trials Ethics Committee (Approval number: GO 21/16, 2021). Research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Consent to Participate
Informed consent was taken from all patients and/or their parents as well.
Consent for Publication
All patients and/or their parents signed informed consent regarding publishing their data.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Süleyman, M., Serin, O., Koçali, B. et al. High Inborn Errors of Immunity Risk in Patients with Granuloma. J Clin Immunol 42, 1795–1809 (2022). https://doi.org/10.1007/s10875-022-01342-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-022-01342-1